اہم نکات
- Peripheral vascular disease (PVD) affects the arteries outside the heart, most commonly in the legs, and can lead to serious complications including amputation if left undiagnosed
- Doppler ultrasound is the primary non-invasive tool for diagnosing PVD, mapping blood flow velocity, waveform patterns, and stenosis locations throughout the lower limb arteries
- The ankle-brachial index (ABI), a simple pressure ratio test, provides the first objective measure of arterial disease and guides whether further Doppler imaging is needed
- Key risk factors include diabetes, smoking, hypertension, and age over 50, all of which are highly prevalent in the UAE population
- Early detection with Doppler allows treatment to begin before complications develop, ranging from lifestyle changes and medication to angioplasty or bypass surgery
Peripheral vascular disease (PVD), also called peripheral artery disease (PAD), occurs when fatty deposits narrow the arteries that supply blood to your legs and feet. The reduced blood flow causes symptoms ranging from leg pain during walking to non-healing wounds and, in severe cases, tissue death requiring amputation. Doppler ultrasound is the frontline diagnostic tool that allows doctors to visualize and measure this arterial narrowing without surgery, radiation, or contrast dye.
Despite affecting an estimated 200 million people worldwide, peripheral vascular disease remains underdiagnosed because its early symptoms are often dismissed as normal aging or muscle fatigue. This guide explains what PVD is, how it develops, why Doppler ultrasound is the preferred diagnostic method, what the test reveals about your arteries, and what treatment pathways are available once a diagnosis is confirmed.
What Is Peripheral Vascular Disease?
Peripheral vascular disease is a circulatory condition in which atherosclerosis, the buildup of fatty plaque inside artery walls, reduces blood flow to the limbs. While PVD can affect any artery outside the heart and brain, it most commonly targets the arteries of the legs: the iliac, femoral, popliteal, and tibial arteries. The disease develops gradually over years, and many patients do not realize they have it until symptoms become significant.
PVD and PAD are often used interchangeably, though technically PVD is a broader term that includes both arterial and venous conditions. In clinical practice, when doctors refer to PVD in the context of atherosclerosis, they are describing the same narrowing process that causes coronary artery disease in the heart, except it is happening in the peripheral circulation. This shared mechanism means that a diagnosis of PVD also signals elevated risk for heart attack and stroke.
Recognizing the Symptoms of PVD
The symptoms of peripheral vascular disease depend on the severity of arterial narrowing and how well the body has developed alternative blood flow pathways (collateral circulation). Many patients progress through recognizable stages as the disease worsens.
Intermittent Claudication
The hallmark symptom of PVD is intermittent claudication, a cramping, aching, or tired feeling in the calf, thigh, or buttock muscles that occurs during walking or exercise and relieves with rest. This happens because the narrowed arteries cannot deliver enough blood to meet the increased oxygen demand of working muscles. The distance a patient can walk before pain begins, known as the claudication distance, is an important clinical measure of disease severity.
Rest Pain
As PVD progresses, pain can occur even at rest, particularly at night when the legs are elevated. Patients often describe a burning or aching sensation in the toes or forefoot that improves when they dangle their feet off the bed, using gravity to assist blood flow. Rest pain indicates severe arterial compromise and requires urgent evaluation.
Skin Changes and Non-Healing Wounds
Advanced PVD produces visible changes in the affected limb: the skin may appear pale, shiny, or discolored; hair loss on the legs and feet is common; toenails become thickened and brittle; and the foot may feel cool to the touch. Most critically, wounds and ulcers on the feet or toes fail to heal because insufficient blood flow prevents the delivery of oxygen and nutrients needed for tissue repair. These non-healing wounds are a major risk factor for infection and potential amputation.
Numbness and Weakness
Reduced blood supply can cause numbness, tingling, or a feeling of heaviness in the legs. In diabetic patients, this symptom can overlap with diabetic neuropathy, making clinical differentiation important. Some patients notice that one leg feels weaker than the other, or that they fatigue more quickly on one side during walking.
The Ankle-Brachial Index: The First Diagnostic Step
Before advanced imaging, the evaluation of suspected PVD typically begins with the ankle-brachial index (ABI), a simple and highly informative test that compares blood pressure in the ankle with blood pressure in the arm. A blood pressure cuff is placed on the ankle and the arm, and a handheld Doppler probe detects the pulse at each location to obtain accurate pressure readings.
The ABI is calculated by dividing the systolic blood pressure at the ankle by the systolic blood pressure in the arm. A normal ABI ranges from 1.00 to 1.40. An ABI below 0.90 confirms the presence of peripheral arterial disease. The lower the ABI, the more severe the disease.
| ABI Value | Interpretation | Clinical Significance |
|---|---|---|
| 1.00 – 1.40 | Normal | No significant arterial narrowing detected |
| 0.91 – 0.99 | Borderline | Possible early disease; exercise ABI testing may be recommended |
| 0.41 – 0.90 | Mild to Moderate PAD | Confirmed arterial disease; Doppler mapping recommended |
| 0.00 – 0.40 | Severe PAD | Critical limb ischemia; urgent vascular assessment needed |
| Above 1.40 | Non-compressible | Common in diabetic patients due to calcified arteries; alternative testing required |
ABI values provide an objective measure of arterial disease severity. Diabetic patients with calcified arteries may show falsely elevated ABI readings.
While the ABI confirms whether arterial disease exists, it does not reveal where the narrowing is located or how extensive it is. This is where Doppler ultrasound becomes essential, providing a detailed map of the entire arterial system from the groin to the feet.
How Doppler Ultrasound Maps Peripheral Arterial Disease
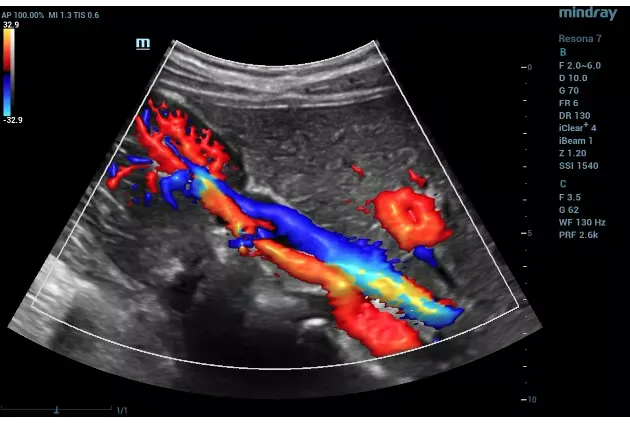
Doppler ultrasound for peripheral vascular disease is a comprehensive examination that traces the arterial blood supply from the aortic bifurcation (where the aorta divides into the two iliac arteries) down through the leg to the foot. The examination combines B-mode (grayscale) imaging to visualize the vessel structure with color Doppler to show blood flow direction and spectral Doppler to analyze flow velocity and waveform patterns.
The sonographer systematically examines the common femoral artery, the superficial femoral artery (the most common site of disease), the popliteal artery behind the knee, and the tibial arteries below the knee. At each level, the examiner looks for plaque, measures vessel diameter, assesses blood flow velocity, and records the Doppler waveform pattern.
Waveform Analysis: Reading the Arterial Signature
One of the most valuable aspects of peripheral Doppler is waveform analysis. In a healthy leg artery, the Doppler waveform shows a characteristic triphasic pattern: a sharp upstroke during systole (the heart's contraction), a brief reversal of flow in early diastole, and a small forward flow component in late diastole. This triphasic pattern indicates a normal, elastic artery with no significant upstream or downstream disease.
As arterial disease develops, the waveform changes progressively. A biphasic waveform (loss of the early diastolic reversal) suggests mild disease or aging-related arterial stiffness. A monophasic waveform (a slow, rounded pattern with continuous forward flow) indicates significant proximal stenosis or occlusion. By reading these waveform signatures at multiple points along the leg, the radiologist can pinpoint the location and severity of disease even before seeing the narrowing directly.
Velocity Measurements and Stenosis Grading
At a point of arterial narrowing, blood velocity increases dramatically as the same volume of blood is forced through a smaller channel. By comparing the peak systolic velocity (PSV) at the stenosis with the PSV in a normal segment just upstream, the radiologist calculates a velocity ratio. A ratio above 2.0 generally indicates at least 50% stenosis, while a ratio above 4.0 suggests stenosis exceeding 75%. Complete occlusion is identified when no flow signal is detected within a visible vessel.
Color Flow Mapping
Color Doppler overlays flow information onto the grayscale image, allowing rapid identification of areas where blood flow is disturbed. Normal arterial flow appears as a uniform color filling the vessel lumen. At a stenosis, the color shifts to indicate higher velocity (typically appearing as a bright alias or mosaic pattern), and beyond the stenosis, turbulent flow appears as mixed colors. This visual map helps the radiologist quickly survey long arterial segments and focus detailed measurements on the areas of concern.
Risk Factors for Peripheral Vascular Disease
Understanding the risk factors for PVD is critical because most of them are modifiable, meaning early intervention can slow or prevent disease progression. The major risk factors overlap significantly with those for coronary artery disease and stroke.
Diabetes
Diabetes is the single strongest risk factor for peripheral vascular disease. People with diabetes are two to four times more likely to develop PVD, and they tend to develop it at a younger age. High blood sugar damages the arterial endothelium (inner lining), promotes inflammation, and accelerates plaque formation. Critically, diabetes also causes peripheral neuropathy, which can mask the pain of claudication, allowing the disease to advance to a severe stage before it is detected. This combination of accelerated disease and reduced symptoms makes Doppler screening especially important for all diabetic patients.
Smoking
Cigarette smoking is the most potent modifiable risk factor for PVD. Smokers are up to four times more likely to develop PAD than non-smokers, and they develop it approximately a decade earlier. Smoking damages the endothelium, increases blood viscosity, promotes clotting, and directly contributes to vasoconstriction. The risk remains elevated even years after quitting, though cessation slows progression and improves treatment outcomes significantly.
Hypertension
Chronic high blood pressure places mechanical stress on artery walls, accelerating the atherosclerotic process. Hypertension increases PVD risk by approximately 50% and makes existing disease more likely to progress. Blood pressure management is therefore both a preventive measure and a core component of PVD treatment.
Age and Other Factors
PVD prevalence increases sharply after age 50, affecting approximately 12% to 20% of adults over 60. High cholesterol, obesity, physical inactivity, chronic kidney disease, and a family history of cardiovascular disease all contribute to elevated risk. Men are affected slightly more frequently than women, though the gap narrows with advancing age.
Treatment Pathways After Doppler Diagnosis
The results of a peripheral Doppler examination directly guide treatment decisions. Management depends on the severity and location of disease, the patient's symptoms, and their overall cardiovascular risk profile.
Lifestyle Modifications
For all stages of PVD, lifestyle changes form the foundation of treatment. Smoking cessation is the single most important intervention, capable of halving the progression rate. Supervised exercise programs, specifically walking programs that push patients to walk through the onset of claudication, have been shown to increase walking distance by 50% to 200% over three to six months. A heart-healthy diet low in saturated fats, regular blood sugar monitoring for diabetic patients, and weight management all contribute to slowing disease progression.
Medical Therapy
Pharmacological treatment targets the underlying risk factors and the disease itself. Antiplatelet agents (aspirin or clopidogrel) reduce the risk of cardiovascular events. Statins lower cholesterol and stabilize existing plaque. Blood pressure medications, particularly ACE inhibitors, provide arterial protection. Cilostazol may be prescribed specifically for claudication, as it improves walking distance by reducing platelet aggregation and promoting vasodilation.
Endovascular and Surgical Interventions
When lifestyle changes and medication are insufficient, or when critical limb ischemia threatens tissue viability, interventional procedures are considered. Angioplasty, where a balloon catheter opens the narrowed artery, often combined with stent placement, is the most common minimally invasive approach. For longer or more complex blockages, surgical bypass grafting, which redirects blood flow around the diseased segment using a vein or synthetic graft, may be necessary. The location and extent of disease identified on the Doppler study are essential for planning these interventions.
PVD in Dubai: A Growing Concern
The prevalence of peripheral vascular disease in Dubai and the wider UAE is a significant public health concern driven by several converging factors. The UAE has one of the highest rates of type 2 diabetes in the world, with approximately 17% of the adult population affected. Given that diabetes is the single strongest risk factor for PVD, this translates directly into elevated disease rates.
Sedentary lifestyles are common in the region, partly driven by the extreme summer heat that limits outdoor physical activity for several months of the year. Combined with the prevalence of high-calorie diets and significant rates of obesity and hypertension, the conditions for atherosclerotic disease are firmly established. The diverse expatriate population also includes large communities from South Asia, where cardiovascular disease tends to present at younger ages.
Despite these risk factors, PVD remains widely underdiagnosed in the region. Many patients attribute leg pain or fatigue to aging, deconditioning, or joint problems rather than seeking vascular evaluation. Increasing awareness of PVD symptoms and the availability of non-invasive Doppler testing is essential for earlier detection and better outcomes.
Peripheral Vascular Doppler at DCDC Dubai Healthcare City
At Doctors Clinic Diagnostic Center in Dubai Healthcare City, peripheral vascular Doppler is performed by experienced radiologists using advanced Doppler ultrasound equipment capable of high-resolution imaging and precise velocity measurements. The examination covers the complete arterial tree of the lower limbs, providing a thorough assessment of disease location, severity, and extent.
The center also offers ABI measurement as part of the vascular assessment, providing a complementary objective measure of overall arterial health. Comprehensive reports include waveform analysis, velocity ratios, stenosis grading, and clinical correlation, all interpreted in the context of the patient's medical history and risk factors. Close coordination with referring physicians, including internists, endocrinologists, and vascular surgeons, ensures that diagnostic findings lead to timely and appropriate treatment decisions.
Experiencing Leg Pain or Numbness?
Peripheral vascular Doppler at Doctors Clinic Diagnostic Center in Dubai Healthcare City can map your leg arteries for narrowing and blockages. Our experienced radiologists provide detailed reports to guide your treatment plan.
Book Vascular Dopplerاکثر پوچھے گئے سوالات
Final Thoughts
Peripheral vascular disease is a common, serious, and underdiagnosed condition that shares its root cause, atherosclerosis, with heart attacks and strokes. The symptoms of leg pain, cramping, numbness, and non-healing wounds should never be dismissed as simply part of aging. Doppler ultrasound provides a painless, radiation-free, and highly accurate method to detect and map arterial disease throughout the legs, giving doctors the detailed information they need to plan effective treatment.
If you have diabetes, smoke or have a smoking history, have high blood pressure, or are over 50 with cardiovascular risk factors, a peripheral vascular Doppler assessment is one of the most valuable preventive steps you can take. Early detection means earlier treatment, better symptom control, and a lower risk of the devastating complications of advanced disease. For pricing details, see our guide on Doppler ultrasound cost in Dubai. At Doctors Clinic Diagnostic Center in Dubai Healthcare City, our vascular imaging team is ready to provide the thorough evaluation your leg health deserves.
ذرائع اور حوالہ جات
یہ مضمون ہماری طبی ٹیم نے جائزہ لیا ہے اور درج ذیل ذرائع کا حوالہ دیتا ہے:
- American Heart Association - Peripheral Artery Disease
- Society for Vascular Surgery - PAD Guidelines
- European Society of Cardiology - PAD Diagnosis and Management
- Radiological Society of North America - Vascular Ultrasound
- International Diabetes Federation - Diabetes and Cardiovascular Disease
اس سائٹ پر طبی مواد کا جائزہ DHA لائسنس یافتہ ڈاکٹرز نے لیا ہے۔ ہماری دیکھیں تحریری پالیسی مزید معلومات کے لیے۔